

Demodex blepharitis is caused by an infestation of Demodex mites, the most common ectoparasite found on humans.1
Many patients have objective signs of Demodex blepharitis, including collarettes, Demodex mites, and lid margin redness.1
Real-world data from a prospective, multicenter, observational study of 311 patients to evaluate the impact of DB.
81% of patients with Demodex blepharitis who were surveyed sought some form of treatment2


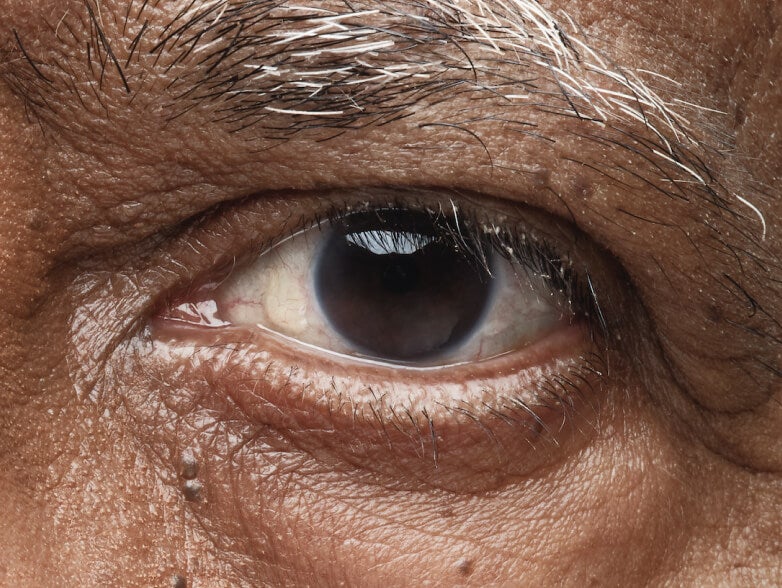







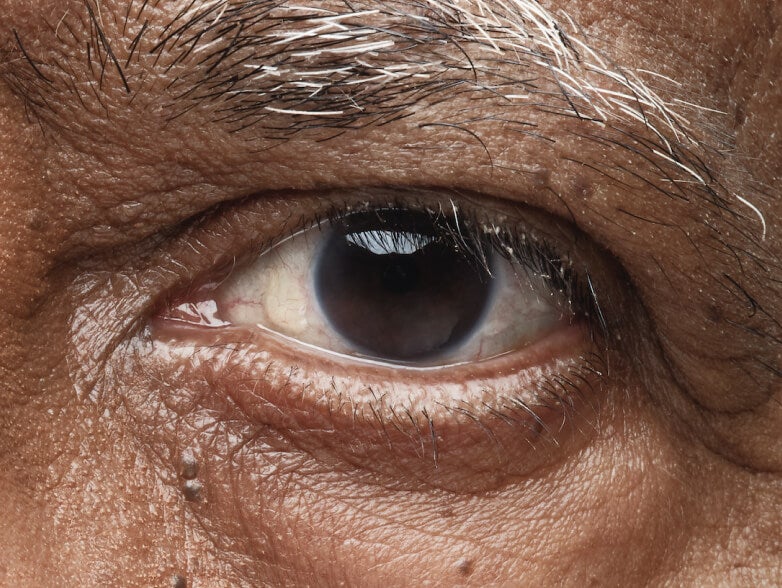





100% of patients with collarettes are found to have Demodex mites. If they have collarettes, then they must have Demodex.3
Collarettes are cylindrical, waxy debris of mite waste products and eggs found at the base of the eyelashes and can be identified during a routine slit lamp exam.1,6
1. Fromstein SR, Harthan JS, Patel J, Opitz DL. Demodex blepharitis: clinical perspectives. Clin Optom (Auckl). 2018;10:57-63. 2. O’Dell L, Dierker DS, Devries DK, et al. Psychosocial impact of Demodex blepharitis. Clin Ophthalmol. 2022;16:2979-2987. 3. Gao YY, Di Pascuale MA, Li W, et al. High prevalence of Demodex in eyelashes with cylindrical dandruff. Invest Ophthalmol Vis Sci. 2005;46(9):3089-3094. 4. Luo X, Li J, Chen C, Tseng S, Liang L. Ocular demodicosis as a potential cause of ocular surface inflammation. Cornea. 2017;36(Suppl 1):S9-S14. 5. English FP, Nutting WB. Demodicosis of ophthalmic concern. Am J Ophthalmol. 1981;91(3):362-372. 6. Bitton E, Aumond S. Demodex and eye disease: a review. Clin Exp Optom. 2020;104(3):285-294. 7. Li J, O’Reilly N, Sheha H, et al. Correlation between ocular Demodex infestation and serum immunoreactivity to Bacillus proteins in patients with facial rosacea. Ophthalmology. 2010;117(5):870-877. 8. Zhu M, Cheng C, Yi H, Lin L, Wu K. Quantitative analysis of the bacteria in blepharitis with Demodex infestation. Front Microbiol. 2018;9:1719.