- Inflammation of the eyelid, conjunctiva, and cornea
- Tearing
- May contribute to recurrent hordeolum or chalazion
- Red and irritated eyelids
- Eyelash misdirection or loss
- Foreign body sensation
- Burning
- Dryness
- Altered meibomian gland function
- Discomfort
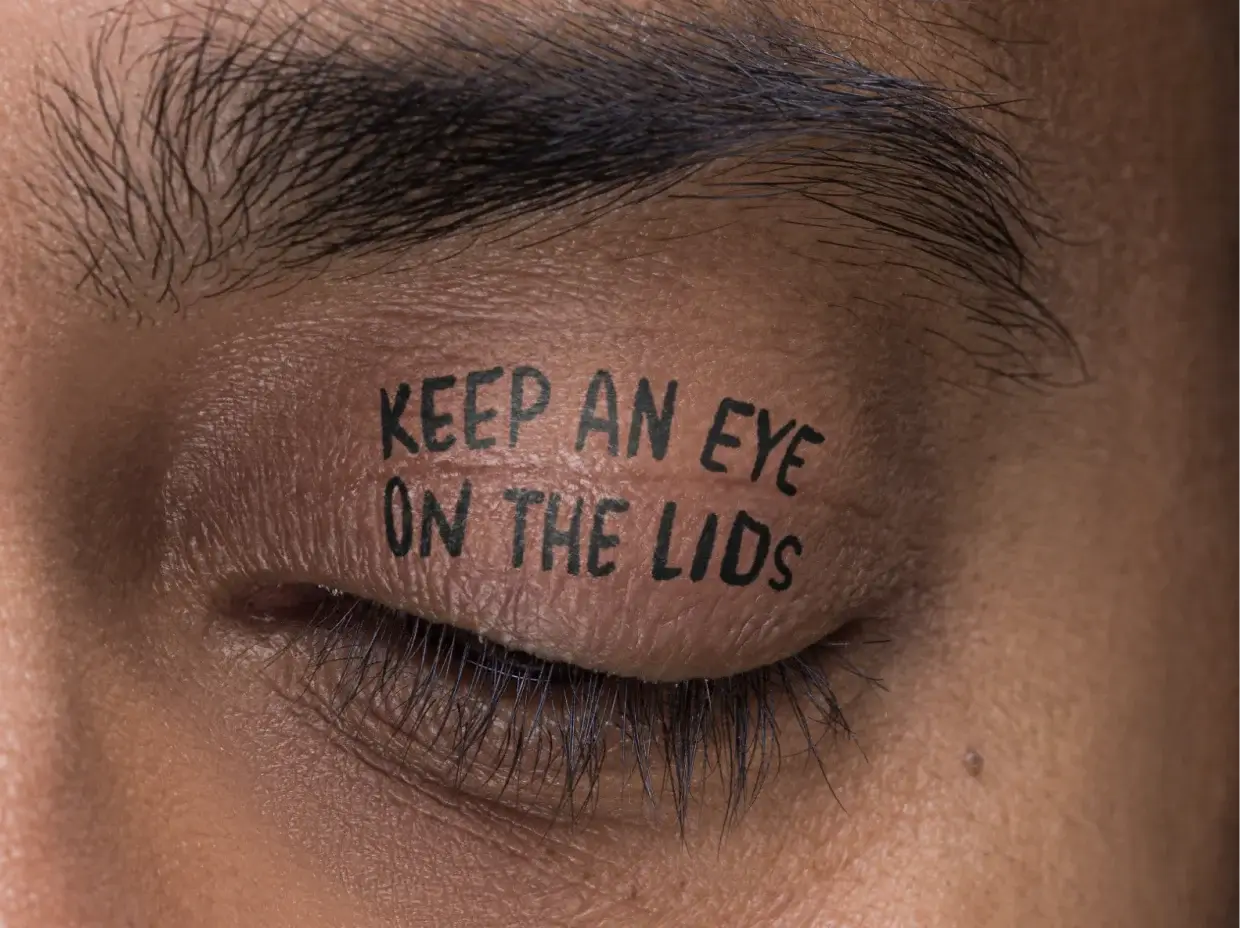
HEMANTH, real patient with DB
Untreated Demodex blepharitis (DB) can have serious consequences
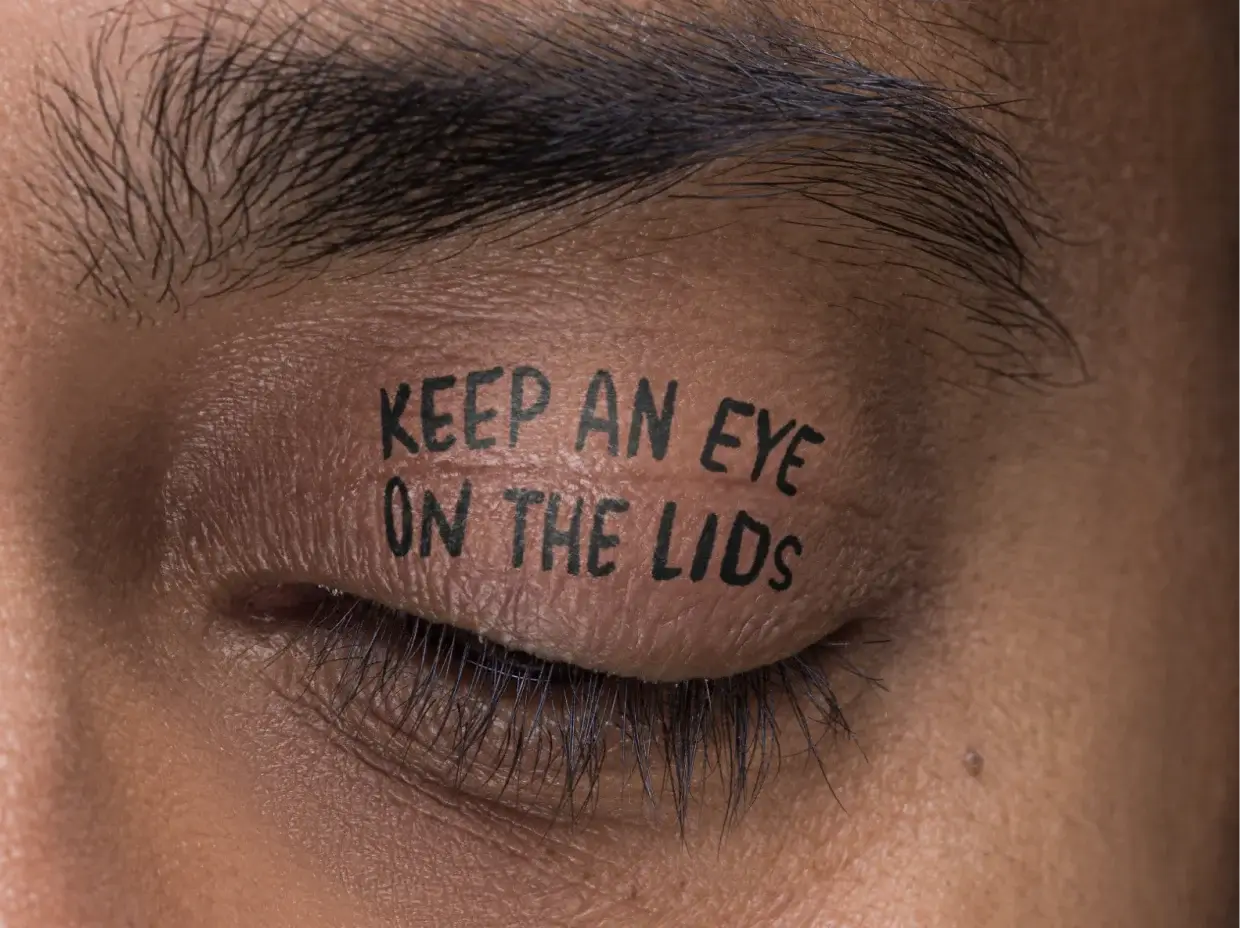
HEMANTH, real patient with DB
DB affects patients physically, functionally, and psychosocially
- Inflammation of the eyelid, conjunctiva, and cornea
- Tearing
- May contribute to recurrent hordeolum or chalazion
- Red and irritated eyelids
- Eyelash misdirection or loss
- Foreign body sensation
- Burning
- Dryness
- Altered meibomian gland function
- Discomfort
- Itching
- Nighttime vision difficulties
- Blurry or fluctuating vision
- Difficulty wearing contact lenses
- Feeling conscious of eyes all day
- Difficulty wearing makeup
- Constant worrying about appearance
One collarette may be just the beginning
DB can trigger new problems for patients — or may make existing problems worse1,4
- ~57% of patients with MGD have DB†
- Through their physical presence in the glands or through inflammation, mites cause:
- Obstruction of gland orifices
- Decrease in meibum quality
- Reduced gland expressibility
- Gland atrophy or loss
- DB is common in surgical candidates
- In a large US clinical study, more than half of the patients presenting for cataract surgery had DB
- DB is associated with increased MMP-9 and reduced TBUT, which may disrupt ocular surface homeostasis and patient satisfaction, particularly for premium IOL implant patients
- Preexisting lid margin disease (blepharitis) is a recognized risk factor for postoperative endophthalmitis after intraocular surgery
- DB prevalence has been reported to increase after cataract surgery, especially following topical steroid use
TBUT=tear break-up time.
- Symptoms from DB and MGD can impact tear film integrity
- A large study found that Demodex-infested eyes had significantly shorter noninvasive tear break-up time, indicating a potentially reduced tear film stability
- In a study to investigate the relationship between Demodex infestation and ocular surface manifestations in MGD (N=86), patients with MGD and Demodex infestation showed higher tear film MMP-9, greater symptom burden (OSDI), and more corneal staining than those without Demodex infestation
- Other studies have shown that patients with Demodex infestation have lower Schirmer test scores and higher OSDI scores than patients without DB
- Wearing contact lenses may increase the susceptibility to Demodex infestation by altering the ocular surface microbiome
- Studies have documented a high degree of overlap between Demodex infestation and soft-contact lens (SCL) intolerance
- Up to 51% of patients wearing SCLs have DB
- ~93% of SCL-intolerant patients had Demodex infestation‡
- Inflammation, excessive keratinization, and hyperplasia of the eyelid epithelium, which can be due to DB, may cause discomfort to the point of lens abandonment
SIGN UP NOW
Be the first to get the latest on DB.